Family Dentistry
When most people think of comprehensive dental examinations, the first thing that usually comes to mind is a checkup. In some cases this is correct. A dental Hygienist might take x-rays, give your teeth a general examination, then clean them. From time to time, however, your Dentist will give you a more comprehensive examination, which will include a look at your entire mouth, head, and neck. He will also probably review your entire medical history, as well as take additional x-rays if he suspects a problem.
Comprehensive examinations are also done frequently when you make your first visit to any Dentist. Even if you have been seeing another Dentist, your new Dentist will want to become familiar with the general state of your health, since this will make it easier for him to notice changes from visit to visit in the future.
The most important part of any visit with your Dentist is your medical history. Whether you are asked or not, you should always let your Dentist know of any health problems you have experienced since your last visit. Even if you don’t think that a problem you have had relates to your mouth, mention it anyway since some diseases can seriously affect your teeth and mouth. Diabetes is a good example of this, since developing diabetes can also lead to periodontal disease. Research has also shown that having periodontal disease can lead to higher blood sugar levels. Periodontal disease can also make diabetes more difficult to treat.
Whenever you see your Dentist, make sure you let them know what medications you are taking as well as dosages since they will need to take that into consideration for some treatments. For example, some health issues will affect the type of anesthesia you can be given. Some medications can cause dry mouth, a problem that can cause an increase in cavities. Knowing what medications you are taken will also alert your Dentist to others he/she might want to prescribe but may cause a negative reaction.
Good comprehensive examinations can go far in assuring you that your Dentist is rendering the best care that can be delivered. Markham Kennedy Dental takes pride in ensuring we do a full work up for each new patient.
Professional teeth cleaning by a certified dental hygienist aims to remove plaque, tarter and stains that have accumulated on the teeth. Even with routine brushing and flossing of your teeth and gums, tarter can develop. The professional cleaning of teeth is a crucial part of good oral hygiene and is needed periodically to maintain the health of your teeth and gums. Most dentists recommend having your teeth professionally cleaned every 6-12 months to reduce the likelihood of periodontal disease progressing. In between routine cleanings, good oral hygiene at home is vital to prevent tarter build-up and gum disease.
Dental cleanings are designed to remove plaque and tarter deposits that have built up on teeth over time. Plaque is the sticky, soft film that contains millions of bacteria. This bacteria found in plaque is what causes gum disease and tooth decay if not removed by daily brushing and flossing, as well as routine trips to the dentist. Tarter, or dental calculus, is a hard calcified deposit that forms on the teeth and can contribute to their decay. Dentists use specialized instruments to gently remove these deposits without causing harm to the teeth. All dental instruments are put through a stringent cleaning, disinfecting, and sterilizing procedure to ensure safety and quality control. A dental mirror will also be used to help the dentist inspect hard-to-see areas in the mouth. Dental mirrors feature elongated handles generally connected to round mirrors. A dental mirror can help the dentist observe the teeth and gums for signs of irritation, swelling, decay, tarter, or bleeding. The first tool that is generally used to clean teeth is an ultrasonic instrument. This device uses mild vibrations to loosen larger pieces of tarter. It also sprays subsequent mists of cool water to wash away loose debris. The tips of the ultrasonic instrument are rounded and curved, and kept in constant motion. The settings on the device can be adjusted for the patient’s comfort.
Once larger pieces of tarter are dislodged, the dentist will make the switch to finer hand-held instruments. Often referred to as curettes or scalers, these tools are designed to eliminate smaller deposits on the teeth and smooth the tooth surfaces. Each tooth must be scaled individually to ensure that all tarter is removed. Once the surfaces of the teeth are smooth, the dentist will polish the teeth. Using a slow-speed handpiece containing a soft rubber cup, the polishing device spins at the tip to smooth teeth. Prophylaxis paste, a gritty toothpaste-like solution, is put into the rubber cup. The cup containing the solution spins on the teeth to create a shiny, smooth surface. In some instances, your dentist may also apply fluoride as the final step in cleaning. Available in a variety of flavors, such as strawberry, chocolate, mint, and cherry, fluoride is placed in flexible foam trays and placed over the teeth. After 30 seconds of the fluoride treatment, the patient is asked to spit the remaining solution into a saliva ejector. Fluoride is used to strengthen teeth and protect them against dental plaque and tarter.
The majority of dental patients find routine teeth cleaning to be painless. The cooling mist of water, mild vibrations, and the pressure felt during “scraping” does not generally caused discomfort. It’s important to let your dentist know if the cleaning is beginning to cause pain, so that they can recommend alterative options to make your teeth cleaning more enjoyable. Most dental cleanings last between 30 minutes to an hour on average, and are performed in a lying position in a comfortable dental chair. After a professional teeth cleaning, you may notice that your teeth feel fresher and look brighter. Teeth cleaning procedures are designed for more than just appearances. Professional teeth cleaning treatments are the primary means of preventing and treating periodontal disease and maintaining tooth health.
Did you know that nearly all adults have had cavities at some point? A staggering 92% of adults between the ages of 20 and 64 have had cavities in their permanent teeth, while 26 percent have untreated cavities. Since cavities are so common, it’s a good idea to offer your employees a dental insurance plan that covers fillings. Many plans cover silver fillings, but not white fillings, which can be confusing for you and your employees.
Here’s what you need to know about silver vs. white fillings so, should you develop a cavity, you can make an informed decision about which type of filling is best for you.
Silver vs. White Fillings: The Basics
Silver-colored fillings—also called dental amalgams—are made of a combination of metals such as silver, tin, copper and mercury. White fillings—also called composite fillings—are made of plastic and ceramic. Both types of fillings can be used to repair cavities, but many dental insurance companies cover only silver fillings. This may concern some employees, but there are good reasons for this policy.
Silver vs. White Fillings: What’s the Difference?
Silver fillings are very durable, so they’re a good choice for teeth that need to withstand a lot of force, such as molars. The material used in silver fillings also hardens more quickly, so it’s easier for dentists to place it in moist areas, such as those beneath the gum line. Silver fillings are also less expensive than white fillings, so they’re good for your bottom line.
The main advantage of white fillings is their color. If you develop a cavity in a highly visible part of your mouth, you may prefer a tooth-colored filling. However, these fillings are weaker than silver fillings and might not last as long. Recurrent decay (the cavities that form underneath a filling) is also a bigger problem with white fillings than with silver fillings.
Choosing Fillings
Some people may be concerned about the fact that silver fillings contain mercury. Rest assured that silver fillings have been used for more than 100 years, and multiple studies have proven that they’re safe. Reputable associations, such as the World Health Organization, the American Dental Association and the Centers for Disease Control and Prevention, all agree that silver fillings pose no risk. This is because the mercury is bound to other metals, which keeps it stable; plus, the mercury in dental fillings isn’t the same kind of mercury (methylmercury) that’s found in tuna or other fish and that can lead to health problems.
Another possible concern is that since silver fillings don’t match the color of your teeth, they won’t look attractive. Fortunately, cavities usually develop in areas that are not readily visible, so the color of the filling isn’t important. While it’s possible to get a cavity on the front surface of a tooth, these surfaces are easy to clean and therefore not prone to cavities. Cavities tend to develop in areas that are hard to clean with a toothbrush, such as the grooves of molars, underneath the gum line or around the edges of crowns.
When a tooth has been damaged by decay or through an accident, rather than remove the tooth completely, it is possible to fit a cover – known as a crown or cap – over the remaining tooth. Under local anesthetic the tooth is reduced in size by the same thickness as the final crown, which will be cemented onto the tooth. An impression of your teeth and gums is then made and a temporary cap is fitted over the tooth until a permanent crown can be made. During your next visit, your dentist will remove the temporary cap and cement the crown onto your tooth.
X-rays allow your dentist to see areas of your teeth and mouth that would otherwise be invisible. Among other things they show cavities between the teeth and infections of the roots. More often than not, small cavities are not visible in the mouth and have absolutely no symptoms. This means that your dentist can detect and treat dental problems before you are even aware of them! If decay and infection go undetected and untreated, they can lead to pain and discomfort as well as more costly and invasive dental treatment. Your dentist will only order X-Rays where there is a diagnostic need and the dentist will order only the type and number of X-Rays that you require. If you have questions about why X-rays are needed, you should talk to your dentist.
At Markham Kennedy Dental Care, we have state of the art digital dental X-Ray machines that not only produce sharp and concise images, but also produce far less radiation than the typical analog X-rays. This means less X-rays for you and more information can be obtained from each image.
You and your dentist may determine that you need a tooth extraction for any number of reasons. Some teeth are extracted because they are severely decayed; others may have advanced periodontal disease, or have broken in a way that cannot be repaired. Other teeth may need removal because they are poorly positioned in the mouth (such as impacted teeth), or in preparation for orthodontic treatment.
The removal of a single tooth can lead to problems related to your chewing ability, problems with your jaw joint, and shifting teeth, which can have a major impact on your dental health. Please discuss with your dentist if your require treatment to replace the missing teeth; these options include: dentures, crown & bridge work, and implants.
A denture is a removable replacement for missing teeth and surrounding tissues. There are two types of dentures available, complete and partial dentures. Complete dentures are used when all the teeth are missing, while partial dentures are used when some natural teeth remain.
Dentures improve your chewing ability by replacing the missing teeth with an acrylic teeth. It improves your chewing and pleasure of eating food. Dentures also provide the visual appearance of having natural teeth, support the lips and cheeks, and correct the ‘collapsed’ appearance commonly seen between the nose and the chin. They help you to speak and pronounce words properly because air cannot escape from the spaces in between your teeth.
However, since dentures are removable appliances, disadvantages are:
- Comfort – some people never get used to wearing dentures full time, the feel of it is not the same as having your own natural teeth
- Appearance – sometimes dentures cannot fully mimic your natural dentition and it can be a cause for embarrassment for some patients so having the right expectations vs reality is important, be sure to speak to your dentist and thoroughly understand the treatment before proceeding
- Cavities – may cause cavities in adjacent teeth if adequate hygiene is not performed
- Injury – may cause soft tissue injury if not adequately adjusted to perfectly fit your mouth. Also after wearing a denture for several years, your bones and gums in your mouth may naturally change causing the denture to fit properly anymore, and therefore can cause sores and discomfort to the oral mucosa.
What are Dental Implants?
Dental implants are metal posts or frames that are surgically positioned into the jawbone beneath your gums. Once in place, they allow your dentist to mount replacement teeth onto them.
How do Dental Implants Work?
Because implants fuse to your jawbone, they provide stable support for artificial teeth. Dentures and bridges mounted to implants won’t slip or shift in your mouth — an especially important benefit when eating and speaking. This secure fit helps the dentures and bridges — as well as individual crowns placed over implants — feel more natural than conventional bridges or dentures.
For some people, ordinary bridges and dentures are simply not comfortable or even possible, due to sore spots, poor ridges or gagging. In addition, ordinary bridges must be attached to teeth on either side of the space left by the missing tooth. An advantage of implants is that no adjacent teeth need to be prepared or ground down to hold your new replacement tooth/teeth in place.
To receive implants, you need to have healthy gums and adequate bone to support the implant. You must also commit to keeping these structures healthy. Meticulous oral hygiene and regular dental visits are critical to the long-term success of dental implants.
Implants are usually more expensive than other methods of tooth replacement, and most insurance carriers typically cover less than 10 percent of the fees.
Has your dentist or endodontist told you that you need root canal treatment? If so, you’re not alone. Millions of teeth are treated and saved each year with root canal, or endodontic, treatment. This page explains root canal treatment in detail and how it can relieve your tooth pain and save your smile.
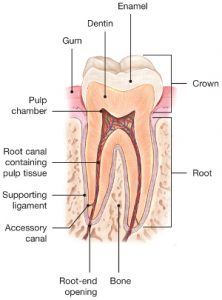
To understand endodontic treatment, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is a soft tissue called the pulp. The pulp contains blood vessels, nerves, and connective tissue and creates the surrounding hard tissues of the tooth during development.
The pulp extends from the crown of the tooth to the tip of the roots where it connects to the tissues surrounding the root. The pulp is important during a tooth’s growth and development. However, once a tooth is fully mature it can survive without the pulp, because the tooth continues to be nourished by the tissues surrounding it.
Endodontic treatment is necessary when the pulp, the soft tissue inside the root canal, becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, or a crack or chip in the tooth. In addition, an injury to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
What are the signs of needing endodontic treatment?
Signs to look for include pain, prolonged sensitivity to heat or cold, tenderness to touch and chewing, discoloration of the tooth, and swelling, drainage and tenderness in the lymph nodes as well as nearby bone and gum tissues. Sometimes, however, there are no symptoms.
How does endodontic treatment save the tooth?
The endodontist removes the inflamed or infected pulp, carefully cleans and shapes the inside of the root canal, then fills and seals the space. Afterwards, you will return to your dentist, who will place a crown or other restoration on the tooth to protect and restore it to full function. After restoration, the tooth continues to function like any other tooth.
Will I feel pain during or after the procedure?
Many endodontic procedures are performed to relieve the pain of toothaches caused by pulp inflammation or infection. With modern techniques and anesthetics, most patients report that they are comfortable during the procedure.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications. Follow your endodontist’s instructions carefully.
Your tooth may continue to feel slightly different from your other teeth for some time after your endodontic treatment is completed. However, if you have severe pain or pressure or pain that lasts more than a few days, call your endodontist.